Provider Sponsored Plans and Medicare Advantage are gaining traction as a critical strategy for profitable, value-based care. However, many underestimate the necessary lead time and effort required to move from consideration to activation. Planning for a 2019 launch needs to begin now starting with a detailed market and organizational feasibility study for standing up a health plan.
Peter Kinhan, Senior Vice President and Market Head
Dan Juberg, Vice President
In recent years, due to increasing cost pressures and competition among providers, many organizations have expressed their ambitions to develop their own health plans, often referred to as provider-sponsored plans (PSPs). Medicare Advantage (MA) is often considered the entry point of choice due to government financial incentives and strong opportunities to drive improvements in both quality and total cost of care for an increasingly aging population.
However, because of competing priorities, many executives struggle to carve out the necessary time to truly evaluate the opportunity. At Lumeris, we believe the time is right to look at MA—in terms of the changing political landscape and the surprisingly lengthy lead times required to assess and apply. This means for those that consider an MA plan as part of their future strategy, that process should start today.
There is no doubt the recent election results have created political uncertainty when it comes to the healthcare industry. There are more things unknown than known. That said, rising healthcare costs are still a major problem to be solved, but value-based care (VBC) has proven to be and will continue to be a critical part of the solution.
So what could change with a new administration and how could it affect your global Medicare strategy? Let’s take note of the significant changes to Medicare that have been gaining traction in the market to date
- MA enrollment continues to grow rapidly. In 2016 there were 17.6 million MA members, which is an increase of more than 200 percent from the number enrolled in 2005.
- MACRA and other CMS programs have deployed value based payment methods that are projected to impact up to 125,000 providers in the traditional Medicare market by 2018.
These two trends demonstrate an important shift to VBC, and if one takes Paul Ryan’s “A Better Way,” as an indication of what is to come from a Republican administration, then it is our opinion the shift will continue—if not accelerate. According to “A Better Way,” Medicare’s “overhaul” would include what Ryan terms “premium support;” a plan to increase competition among providers and allow beneficiaries the freedom to choose where to spend their healthcare dollars. Sometimes called a defined contribution or voucher system, the desired effect of this approach would be to push Medicare further away from its current largely fee-for-service setup by providing increased incentives for beneficiaries to be cost-conscious in their plan selection.
This would likely drive a considerable enrollment increase in the already-growing private MA market; a space that has long been a strong component of Republican plans. As Medicare grows and seeks to control costs, providers can expect a doubling down of population health and a need for health systems to capture a larger share of the premium dollar. MA has always been a critical aspect of organizations’ population health strategy, and with the political changes, we believe that need and opportunity has only strengthened.
Many organizations have been preparing for a migration up the Medicare food chain through the creation of their own health plan. According to Avalere, providers are leveraging their large integrated delivery networks to establish plans at an increasing pace, representing 58 percent of new MA plans entering the program in 2016. Many of these organizations have been developing the necessary competencies by establishing risk-bearing Accountable Care Organizations (ACOs) or accepting delegated risk. Many are confronted with familiar dilemmas. What are the next steps as these ACO agreement periods wind to a close? If launching an MA plan is a couple years down the road, when is the right time to start the “two years from now” process?
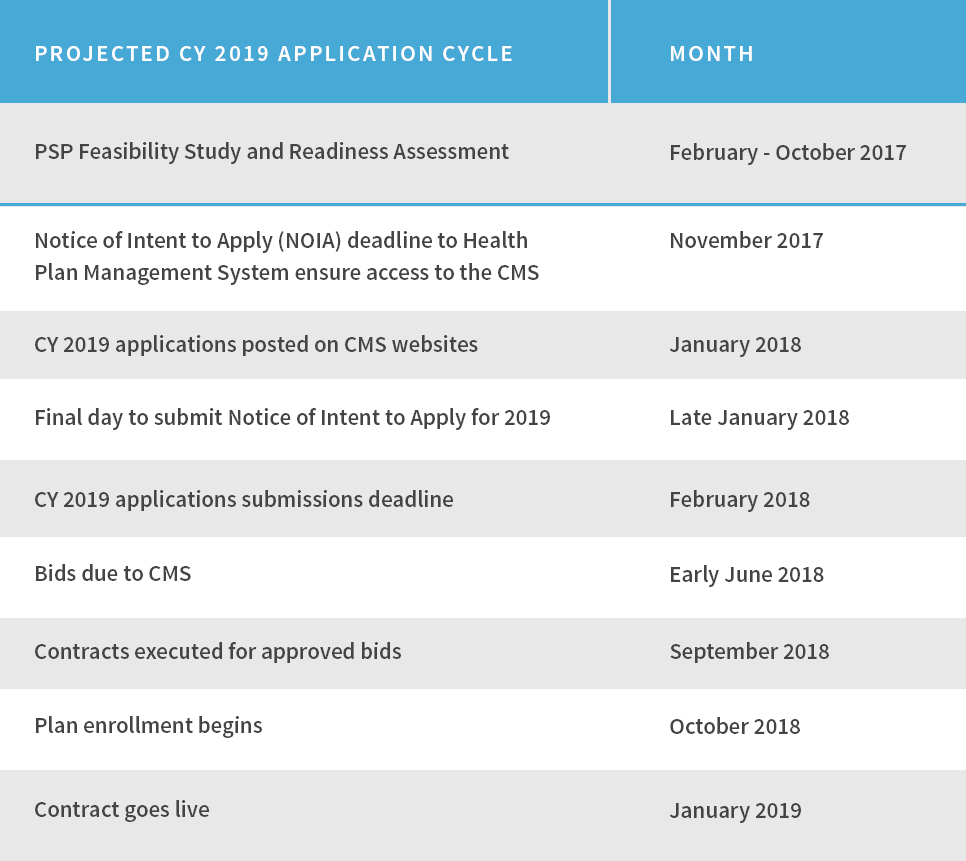
The MA application process differs greatly from the Medicare ACO application process and it starts roughly six months earlier. This is a significant undertaking with great opportunity, and large risk. It requires an in-depth analysis and planning and the necessary time to align organizational strategy.
The Notice of Intent to Apply for a 2019 Medicare Advantage contract opens in mid-November 2017. However the real work should begin much earlier than that. A candid evaluation of whether your organization is ready to run its own health plan takes time and thoughtful consideration. And the question isn’t simply just “Can we?” Of equal importance is “Should we? Will the market support it? Will we need partners or help? What kind of optionality should we be considering and planning for?”
Organizations legitimately contemplating starting an MA plan are taking a deep dive to assess their organizational and network readiness, scope out their competitive landscape and determine not only the overall opportunity present in the market but the viability of their organization being able to capitalize on it. We at Lumeris call this a PSP Feasibility Study, and it’s a crucial first step to setting the wheels in motion for a successful and targeted health plan application and development process.
Key deliverables of a PSP Feasibility Study include:
- Market Assessment;
- Prospective Partner List;
- Network Adequacy Analysis;
- Go-To Market Product and Network Structure;
- Target Market Landscape and Competitive Positioning Strategy;
- Organizational Readiness; and
- Financial Pro Forma.
Armed with an honest assessment of the critical factors to successfully stand up and operate a health plan, organizations not only better understand their readiness but are also able to act immediately to implement any necessary improvements. Providers should be aware of specific opportunities available, and precisely what it will take for them to actualize them.
As a result of this PSP Feasibility Study, the executive team will be better informed for the ultimate decision as to whether they should pursue an MA contract. Should a “go” decision result, progressive organizations should then work to develop an implementation plan in tandem with the application process. While the development of a health plan has never been considered easy, this only underscores just how much preparation many successful organizations undergo.
With so many competing initiatives and so much uncertainty in healthcare right now, it can be easy to overlook or delay the analysis of your MA opportunity. However, we contend that with the political changes and continued demographic evolution, it has never been more important to assess this opportunity—and that process needs to start soon if organizations want options for 2019.
To learn more about conducting a PSP Feasibility Study for your organization, please contact Dan Juberg at djuberg@lumeris.com.


