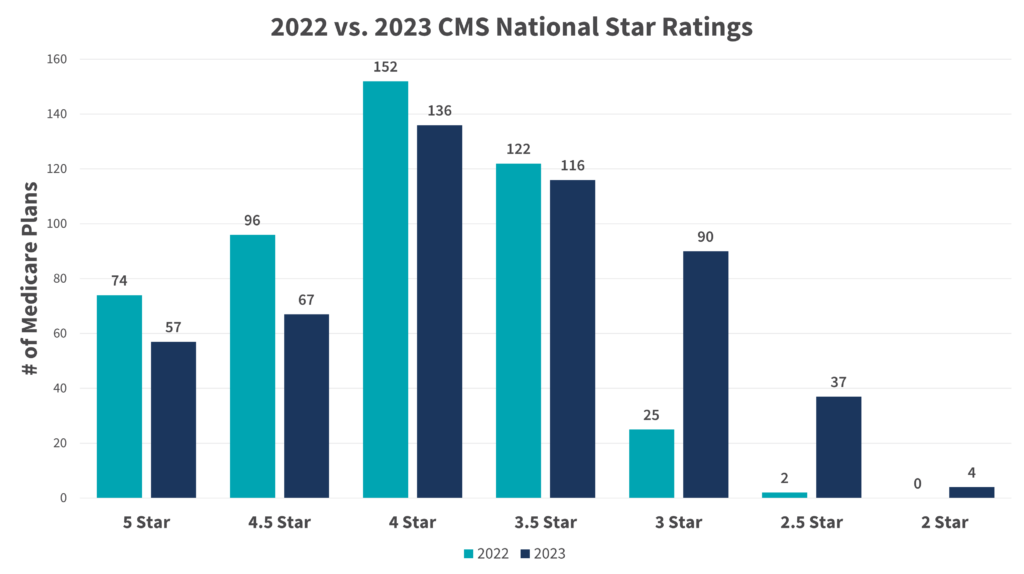
Our organization was founded on the belief that a sustainable model for value-based care is possible along with a deep commitment to achieving the highest quality of care and the best consumer experience while lowering medical spend. This year Essence Healthcare—owned and operated by Lumeris—for the second year in a row achieved the highest Overall Plan Rating of 5 stars for 2023 by the Centers for Medicare & Medicaid Services (CMS). We are particularly proud to have received a raw score of 5.115 from CMS, bucking the national downward trend in Star ratings and achieving an average of more than 4.5 stars for 13 straight years.
Measuring Excellence: The Five-Star System
Annually, CMS releases Star Ratings to reflect the experiences of people enrolled in MA plans. Plans are rated on a one-to-five scale, with one star representing poor performance and five stars representing excellent performance. CMS adds a “reward factor” that’s worth up to 0.4 points for plans that are consistently high performing across all the measures they assess. Essence Healthcare was in the very top percentile on both overall score and variability this year, resulting in a rating that exceeds 5 stars.
Factor 1: Data Analytics Drives Excellence in Star Measures & Enhanced Patient Experience
The growing demand for value-based, patient-centric care has resulted in a considerable shift towards the use of predictive and preventative measures when it comes to public health in recent years. Essence realized early on the impact data analytics can have on both the patient experience and patient outcomes. Utilizing technology and operational model powered by Lumeris, Essence provided their physician partners with combined descriptive (historical data used to identify patterns) and predictive analytics capabilities to help drive real-time clinical decisions to close gaps in care which led to improved outcomes and excellent performance ratings across several CMS quality measures.
For example, using this data-driven technology enabled physicians to better co-manage patients’ diabetes care specific to blood sugar control, leading to an increase in Essence’s “diabetes care: blood sugar control” score from a 5 star score of 88% in 2021 to 88% in 2022, and 93% in 2023.
Factor 2: Physician Engagement & Support
Critical to Essence’s performance is the level of provider engagement and commitment to work together to fully realize the promise and delivery of quality value-based care. Key components of support to drive physician engagement:
- Physician group incentives around a subset of Star measures
- A team to support the providers in implementing programs at the group and the office level
- Consistent provider/practice education and training
- Collaborative provider structure that includes clinical and administrative support
- Technology powered by Lumeris that helps physicians identify actionable health opportunities to optimize care utilization and reduce cost over time
- Value-based programs aligned with physician incentives
Through highly collaborative physician engagement, Lumeris assessed, designed, and deployed best-practice workflows and programs that assisted in moving each Essence physician partners’ practices along the value-based care continuum.
Factor 3: Member Engagement Leads to Better Experience & Outcomes
Essence’s 2023 score demonstrates how the proper rigor around these critical factors can yield extraordinary results, including perfect member experience scores that include both health plan operations and their experience with the care delivery system—a testament to the Lumeris model of collaborating with physicians. In addition to receiving a perfect 5 star rating in the member experience domain, Essence also received 5 stars in the following domains:
- Staying Healthy (Screenings, Tests and Vaccines)
- Managing Chronic (Long-Term) Conditions
- Member Experience with Drug Plan
- Member Experience with Health Plan (additionally, overall plan rating scored 5 stars consecutively from 2019 to 2023)
- Health Plan Customer Service
Having high levels of member engagement was critical for Essence in receiving its 5 star rating—not just in the member experience domain, but as a contributing factor to every CMS quality measure. The more engaged members are in co-managing their health with their providers, the better the outcomes.
Factor 4: Clinical Programs that Keep Patients & Their Health on Track
Lumeris provides Essence’s physician partners with a platform that enables clinical insights from data analytics, population health capabilities, and AI-driven clinical programs. These capabilities help physicians and patients maintain appropriate levels of communications based on health needs and facilitate better health management by both parties. Physicians can access insights to make clinical decisions on the best next steps of care while patients can stay in touch with their providers by opting to receive health alerts and reminders.
Essence physician partners currently have access to more than 10 clinical programs, most of which align with the CMS quality measures.
Factor 5: Operational Excellence is the Baseline for Year-Over-Year Success
What pulls all the factors of success together is having a proven operational model—equal parts the right strategy and the right people—to deploy value-based care in a way that can be replicated easily year after year.
Building Upon Proven Success
Maintaining 5 stars for multiple years in a row requires year-over-year improvement. As we look to create the system of care every doctor wants for their own family, it is critical that we continue to identify new ways to improve upon the current system of care delivery. Through data analytics, physician engagement, member engagement, clinical programs, and operational excellence, it is possible to attain that improvement.
A sustainable model for value-based care is both possible and real today. Lumeris is currently creating that reality in 15 markets, impacting more than one million lives under value-based contracts. With Lumeris as a partner, health systems across the country are fulfilling the promise of value-based care.
