In a recent webinar hosted by the American College of Healthcare Executives (ACHE), Lumeris’ own Rick Goddard was joined by Jeff Anderson of Lifepoint Health to explore how health systems can effectively foster successful payer partnerships to ensure sustainable financial success in value-based care. In this blog, we will summarize this important conversation to shed light on the key competencies needed to navigate the complex healthcare landscape through aligned incentives that work for both payers and providers.
The dynamics between payers and providers must evolve from transactional to strategic as we transition to a value-based payment model. Collaboration is essential to thrive in an increasingly competitive and resource-constrained environment. In this webinar discussion, four key strategies for “winning together” were discussed such that health systems can cultivate effective value-based payer partnerships for a more sustainable financial future.
Value-based contracting is not a zero-sum game. There is an opportunity for both parties to get what they want, but this mindset needs to come from the beginning.
STRATEGY #1: Understanding the Payer Perspective
Health system reliance on commercial fee-for-service revenue is not sustainable.
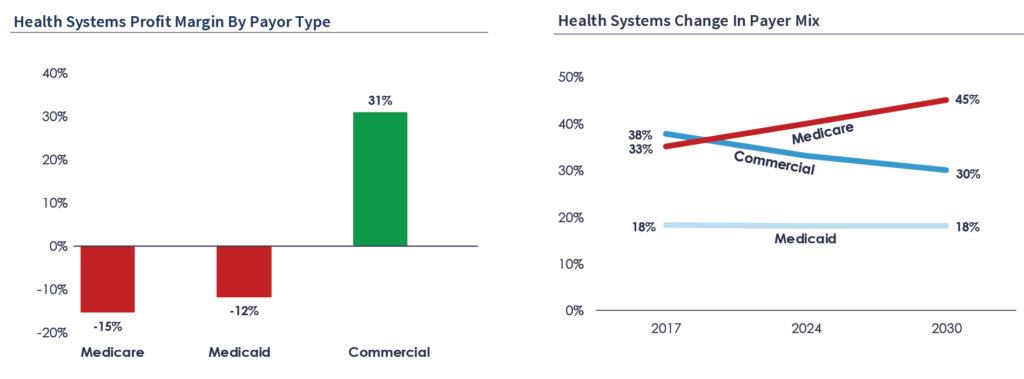
Visual content from recent ACHE Webinar: “Winning Together: Navigating Payer Partnerships for a Sustainable Financial Future”
Similarly, payers are facing significant PMPM revenue and cost headwinds.
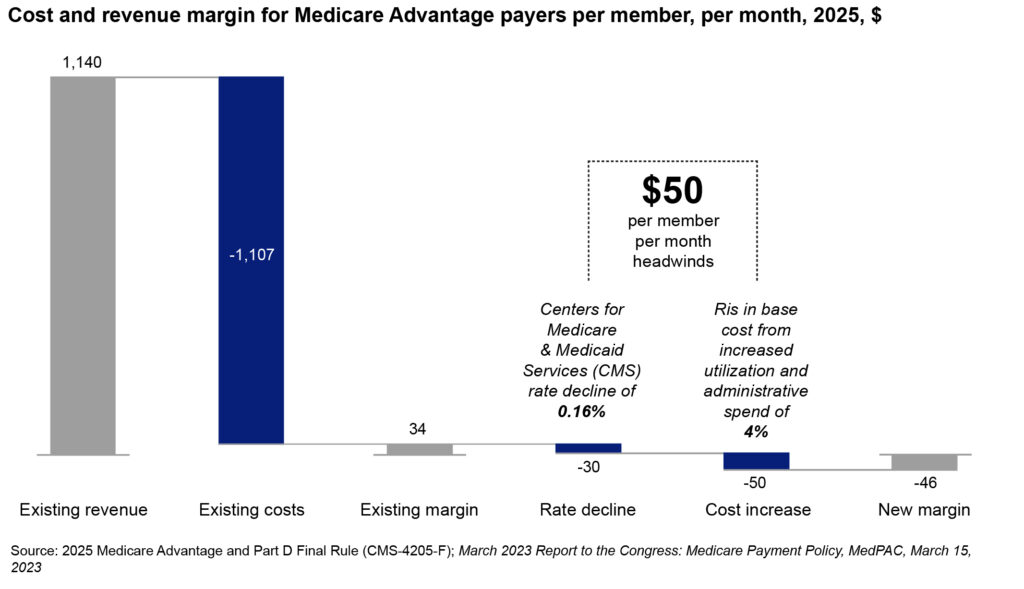
Visual content from recent ACHE Webinar: “Winning Together: Navigating Payer Partnerships for a Sustainable Financial Future”
In today’s healthcare landscape, both health systems and payers are experiencing significant compression on their operating margins. In such a distressed business climate, provider-payer partnerships in value-based care can no longer be personified by short-term contractual negotiations or isolated initiatives. Instead, these two parties must work together toward shared outcomes that are sustained in the long-term to ensure financial sustainability. This shift requires an understanding of payer priorities and operational frameworks, especially as value-based care contracts become the dominant model. Key to this understanding is recognizing that providers must develop competencies that go beyond clinical care, such as risk management, population health, data analytics, and risk underwriting. These capabilities are crucial for engaging meaningfully in value-based agreements that reward quality over volume.
If you're a health system with expensive assets, be aware of what’s happening around you in terms of local payer-owned providers and value propositions.
STRATEGY #2: Building a “Payvider” Skillset
You don’t have to be a payer to think like a payer, or a provider to think like a provider. Both parties need to meet in the middle with empathy and tactical thinking to achieve shared value.
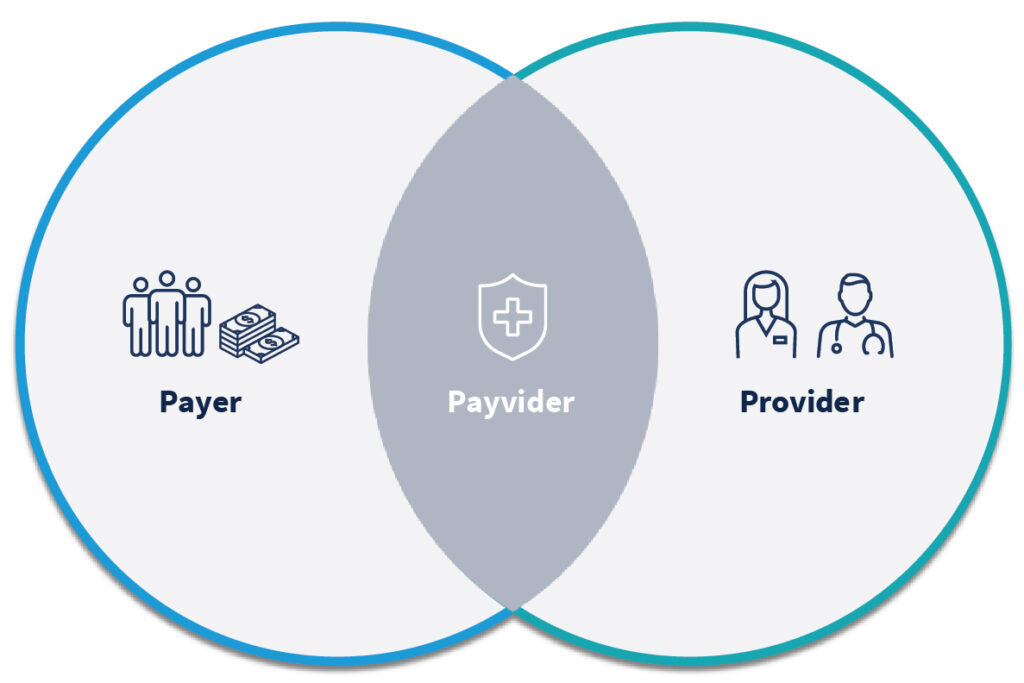
Visual content from recent ACHE Webinar: “Winning Together: Navigating Payer Partnerships for a Sustainable Financial Future”
To truly succeed in value-based contracts, providers must develop a “payvider” skillset. This includes honing negotiation strategies and understanding the financial implications of shared risk arrangements. Key to this approach is a comprehensive knowledge of attribution, utilization management, and care delivery outcomes. Providers who can anticipate and address payer concerns—such as quality star ratings for Medicare Advantage plans, reducing medical loss ratios (MLR), and accurate risk adjustment scores—are better positioned to secure favorable contracts that balance risk and reward.
Health systems that develop these skills allow providers to act as both healthcare deliverers and financial stewards (hence the term “payvider”). Providers who can anticipate payer needs will be in a stronger position to negotiate favorable contracts. It’s no longer sufficient to focus solely on the traditional fee-for-service metrics. Instead, healthcare organizations must take an active role in understanding the financial underpinnings of payer models, aligning their strategies with payer incentives while maintaining clinical excellence.
Central to this transformation is the ability to harness data effectively. Data transparency, sharing, and utilization form the backbone of any successful payer-provider collaboration. To thrive in value-based care arrangements, both parties need to share timely, accurate data to monitor performance, address inefficiencies, and optimize outcomes. This data not only drives decision-making at the provider level but also informs payers about the effectiveness of care delivery and risk management strategies. A truly collaborative relationship hinges on this exchange, as it allows both parties to adapt to changing conditions, optimize care delivery, and mitigate financial risks.
Be prepared—come with market research, know exactly what their situation is, and identify the key levers they need to improve, such as annual wellness visit numbers.
The payer should want to work with you because helping them improve star ratings and managing utilization also improves your position. It’s about finding alignment in performance and goals.
STRATEGY #3: Collaborative Relationships for Long-Term Success
What does a collaborative relationship with a payer look like? How can health systems forge long-term partnerships that are equitable to both parties in the long-term? (Hint: It all comes down to trust.)
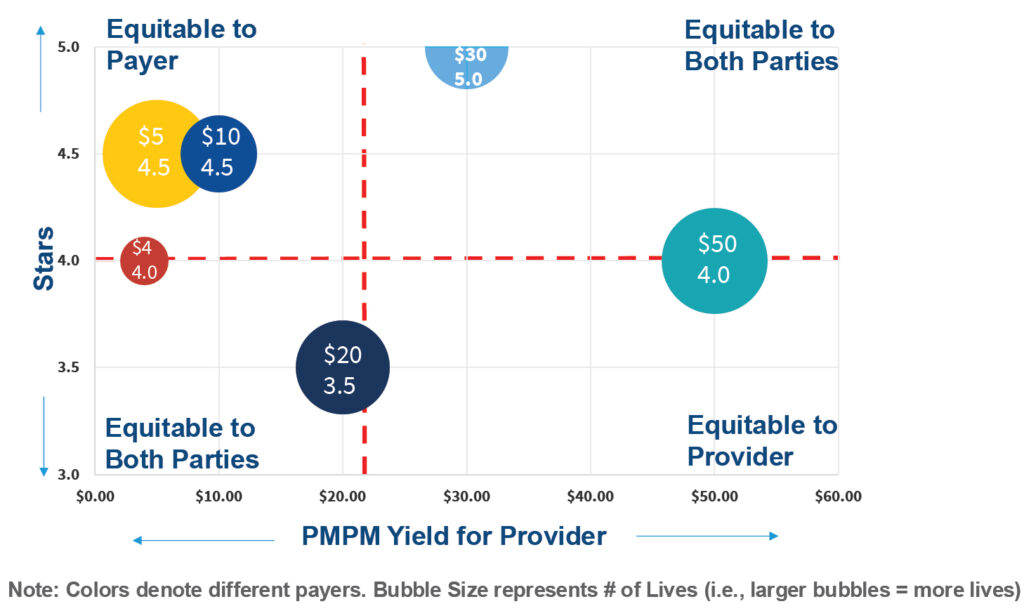
Visual content from recent ACHE Webinar: “Winning Together: Navigating Payer Partnerships for a Sustainable Financial Future”
Trust is the cornerstone of effective payer-provider partnerships. Historically, these relationships have been transactional, often characterized by conflict over reimbursement rates and contract terms. Moving forward, trust and transparency must take precedence. Providers should approach these relationships with a clear understanding of the value they bring, such as their ability to improve patient outcomes, manage chronic conditions, or reduce avoidable hospitalizations. Meanwhile, payers must recognize the essential role providers play in delivering high-quality, cost-effective care. Only through open communication and a shared commitment to patient outcomes can both parties achieve long-term success.
One of the more innovative approaches to fostering payer-provider alignment that ensures trust and transparency is through joint ventures. These partnerships offer the potential for deeper integration, enabling both payers and providers to share risks and rewards. Joint ventures allow for a more comprehensive approach to managing population health, as they bring together the strengths of both entities—payers’ financial management expertise and providers’ clinical care capabilities. The success of these arrangements, however, depends on clear governance structures, financial transparency, and a shared vision for growth. By jointly managing patient populations, payers and providers can create value not only for themselves but also for the patients they serve.
There has to be transparency and trust in data sharing. Both parties should enter long-term relationships based on open communication and shared goals.
The joint venture model is highly collaborative. Both parties need to know each other’s goals and you win or lose together.
STRATEGY #4: Invest in a Culture of Care Delivery Transformation
Transforming a health system to succeed in value-based care requires a shift in culture and mindset. Providers must focus on quality improvement, preventive care, and patient-centered strategies, all while maintaining financial viability. Developing network “mindshare is crucial to this transformation. This means engaging both employed and independent physicians in the network, ensuring they understand and are committed to the principles of value-based care, but also have a sufficient weight of their panel mix include patients attributed to value-based contracts. Care delivery transformation involves not only educating providers about the financial and clinical benefits of population health management but also equipping them with the tools and data necessary to track and improve patient outcomes.
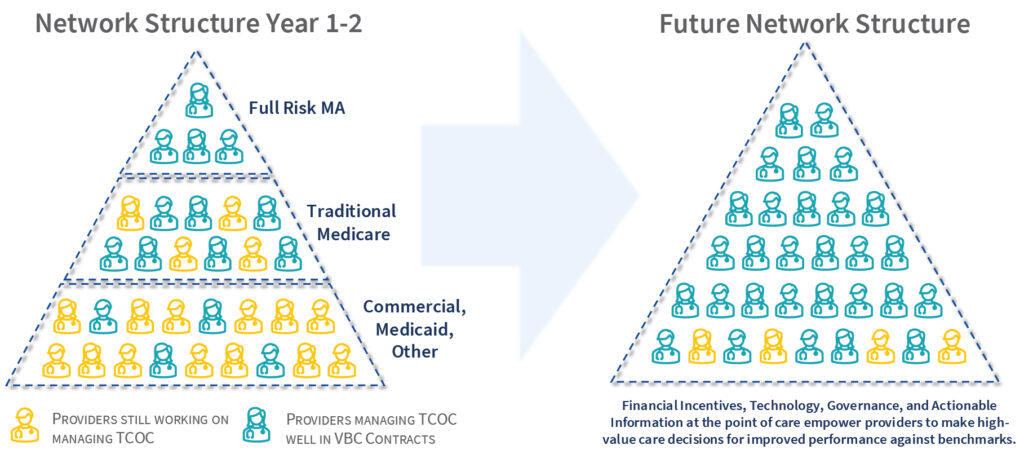
Visual content from recent ACHE Webinar: “Winning Together: Navigating Payer Partnerships for a Sustainable Financial Future”
Payer-provider collaboration in the Medicare Advantage (MA) space can accelerate care delivery transformation. As MA enrollment continues to rise, providers are increasingly exploring opportunities to take on more financial risk in exchange for a greater share of the premium dollar. However, the path to risk should be gradual. Providers must first build capabilities in areas like quality metrics, patient engagement, and preventive care before fully embracing capitated or shared-risk models. By starting with smaller, performance-based contracts and progressively assuming more responsibility, providers can position themselves to capture greater shared savings and improve their financial performance without overwhelming their operational infrastructure.
While the opportunities for collaboration are clear, the challenges remain significant. Providers must move beyond the mindset of being passive participants in value-based contracts and instead take a leadership role in shaping these agreements. This involves understanding not only their own capabilities but also the market dynamics that influence payer behavior. For example, payers may face quarterly earnings pressures or regulatory changes that affect their willingness to share risk or negotiate favorable terms. Providers who can bring market insights to the table and present solutions to these challenges are more likely to succeed in securing advantageous contracts.
Payers should want to work with you and make you successful, especially when starting with Medicare Advantage. Starting small with shared savings can gradually engage physicians and build momentum.
Winning Together for a Sustainable Financial Future
Payer-provider collaboration in value-based care is not a zero-sum game. Both parties have much to gain by working together to improve patient outcomes while controlling costs. For healthcare organizations, this means investing in the infrastructure needed to manage risk, analyze data, and coordinate care effectively. For payers, it means recognizing that providers are essential partners in driving quality and efficiency. Through trust, data sharing, and a shared commitment to patient health, payers and providers can create sustainable models that benefit not only their organizations but also the communities they serve.
To learn more about this important topic, register now to attend ACHE’s 2025 Congress on Healthcare Leadership! Rick and Jeff will be revisiting this topic much more in depth during a panel discussion that also includes Dr. Luis Garcia (President, Rush Medical Group) and Patrick Young (President Population Health, Hackensack Meridian Health).
