The nation has been in a state of healthcare crisis following the pandemic and perhaps the worst hit are rural health organizations. From 2005-2022, a whopping 186 rural hospitals have closed, of which 47 closings occurred from 2019-2022.
As rural hospitals continue to shutter, physician practices are left carrying the responsibility of caring for the communities. Physicians in rural America provide healthcare to ~46 million patients, and with sicker patients, greater administrative burdens, worsening physician payments, and ongoing battles with insurers, these providers are understandably burnt out.
The Unique Strengths and Challenges of Rural Healthcare
There are several key strengths and challenges that set rural health organizations apart from their urban counterparts.
Strengths |
|
Challenges |
|
Perhaps one of the greatest challenges with patient care in rural communities is managing high-risk patients. Many rural patients face challenges with accessing timely care, which further exacerbates their health conditions and poses an additional obstacle for the providers managing their care. As a result, there is a significant disparity between urban and rural populations when it comes to chronic disease prevalence and outcomes. Chronic disease-related rates of death per 100,000 for rural communities were 38% higher for chronic lower respiratory disease, 17% higher for heart disease, 15% higher for stroke, and 10% higher for cancer than in urban communities.
Unfortunately, it is difficult for these providers to care for high-risk patients under FFS arrangements due to increased patient volumes and limited resources. Conversely, value-based care reduces patient volumes by prioritizing appropriate utilization and enabling providers to devote more time and resources to the highest risk patients. Since value-based reimbursement is closely tied to quality of care and patient outcomes, providers can both improve the health outcomes of their patients and enhance their own reimbursement under this model of care.
Rural health organizations can realize substantial value from value-based arrangements by leveraging their unique capabilities and partnering with like-minded organizations that can provide access to:
- Predictive analytics to prioritize high-risk patients
- Accurate documentation and coding support to ensure appropriate reimbursement
- Virtual care resources that allow providers to reach a larger patient population
How Value-Based Care Can Help Rural Organizations Achieve Financial Sustainability
Medicare physician payment, alone, has fallen 29% since 2001, and as FFS reimbursement continues to decline in a world with rising costs, it is imperative for rural health organizations to explore alternative options. For rural organizations that are barely breaking even, or more likely, operating in the red, cuts to reimbursement that affect a large portion of their panels is detrimental.
Value-based care (VBC) offers a solution to physicians that are looking to diversify their FFS revenue and care for their patient panels, while remaining financially viable.
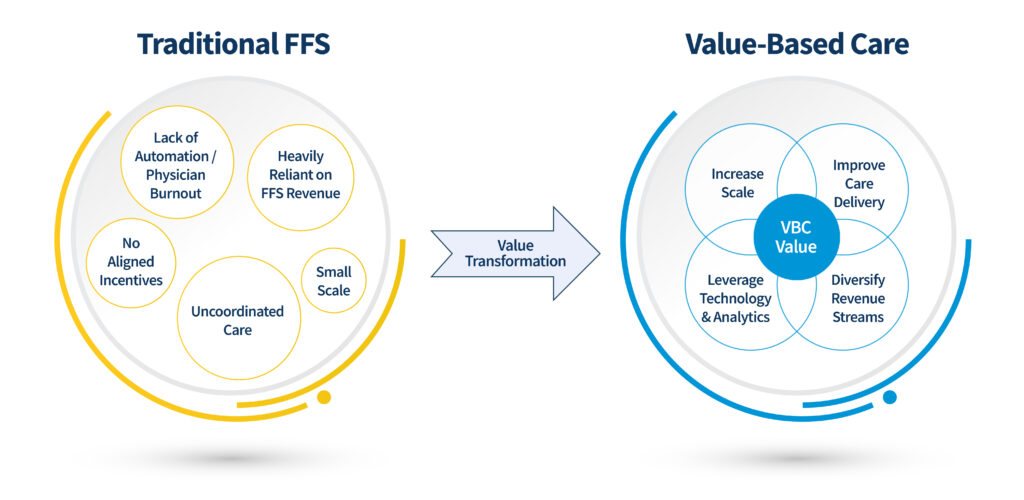
- Increasing Scale
- Since many rural healthcare organizations are smaller in size and may face significant downside risk exposure in value-based care arrangements, creating a network with other like-minded organizations allows rural health organizations to meaningfully partake in VBC with less risk exposure
- VBC Revenue Streams
- Instead of relying purely on FFS reimbursement, setting up value-based care payer contracts and/or participating in a CMMI program with potential shared savings, provides multiple streams of revenue to drive the financial success of the organization
- Care Delivery Transformation
- By improving closing gaps in care, identifying high-risk patients, and directing patients to appropriate sites of care, organizations can reduce unnecessary utilization and improve patient health outcomes
- Technology & Analytics
- Technology is a powerful tool for tracking quality metrics, engaging with patients, reducing administrative workload for providers, and identifying trends or opportunities in the data to implement specific workflows/initiatives
To succeed in value-based care it is important to have the right financial, operational, and care transformation resources in place, that are working in unison, to improve the patient population’s health outcomes.
As CMS forges forward with its goal to have 100% of Medicare beneficiaries and a majority of Medicaid beneficiaries in accountable care by 2030, it is an opportune time for rural organizations to make a shift towards value-based care and take advantage of programs designed to support organizations with fewer resources, such as the ACO Primary Care FLEX (ACO PC Flex) model or the Making Care Primary (MCP) model. These models recognize the unique challenges that smaller healthcare organizations face and provide upfront capital to fund necessary infrastructure investments.
- ACO Primary Care FLEX (ACO PC Flex)
- The ACO PC Flex Model is a five-year voluntary model within the Shared Savings Program that begins January 1, 2025.
- This model specifically targets low revenue ACOs that are typically comprised of smaller hospitals or serve rural communities.
- The model’s new monthly Prospective Primary Care Payment (PPCP) will provide an upfront payment to enhance the predictability and amount of primary care funding for low revenue ACOs, thus increasing their flexibility to meet the needs of people with Medicare.
- The model also includes a one-time, $250,000 Advanced Shared Savings Payment to help cover costs associated with forming an ACO and administrative costs for model activities.
- Making Care Primary (MCP)
- The Making Care Primary (MCP) Model is a 10.5-year multi-payer model with 3 participation tracks designed to support an organization’s transformation to VBC, from building infrastructure to optimizing care.
- Organizations typically eligible for this program include independent practices, Indian Health programs, FQHCs, group practices, health systems, and certain critical access hospitals.
- Practices starting in Track 1 of MCP focus on building infrastructure for advanced primary care, including risk stratification and chronic disease management. They receive fee-for-service payments with additional financial support to develop their care capabilities.
- Track 1 participants may receive $72,500 in a lump sum payment at the start of Year 1 and an additional $72,500 at the start of Year 2 as an Upfront Infrastructure Payment (UIP).
Why is the Shift to Value-Based Care Important?
Serving rural communities requires innovative solutions that consider the unique challenges that impact rural America today. At the current rate, reliance on FFS reimbursement will likely lead to more hospital closures and widened care gaps. However, substantial value can be unlocked by equipping rural healthcare providers with the tools and resources needed to manage patient care and partaking in alternative payment options to boost revenue.
Now more than ever, America’s rural communities cannot afford to lose physicians to urban regions or see their nearest hospital close down. As America’s aging population increases, with nearly 25% of seniors residing in rural communities, access to high quality care in rural America is paramount.
As rural health organizations navigate the unprecedented challenges of our time, the shift to value-based care offers a lifeline. Value-based models empower these organizations to provide more sustainable and high-quality care for rural communities by focusing on long-term health outcomes and the holistic well-being of their patients, ensuring that even in the face of adversity, rural America receives the care it deserves.

