The Centers for Medicare & Medicaid Services (CMS) has released the 2023 performance results for both the ACO REACH Model and the Medicare Shared Savings Program (MSSP), showcasing the ongoing impact of value-based care in enhancing health outcomes and generating significant savings. These results reflect a crucial milestone in the movement toward accountable care, models designed to empower healthcare providers to deliver patient-centered, coordinated care. At Lumeris, we’re honored to support health systems and practices across the country in navigating this journey, providing the tools, expertise, and technology to enable sustainable success in value-based care.
In this blog, we provide an in-depth look at what you need to know about both ACO REACH and MSSP’s PY2023 results, highlighting key achievements, financial and quality improvements, and the importance of these programs in shaping a more equitable and efficient healthcare landscape. Whether you are part of an ACO or exploring value-based models, understanding these results can inform your strategy and inspire further progress in transforming patient care.
ACO REACH Model: Performance Year 2023
The recent announcement from CMS on ACO REACH confirms that the model is making a remarkable impact. In Performance Year 2023, it clearly demonstrated its potential to promote health equity, expand access, and empower community health – all while reducing healthcare costs and improving outcomes. REACH ACOs generated substantial savings and quality improvements, with CMS reporting approximately $1.643 billion in gross savings. This result represents a 5.8% gross savings rate relative to the retrospective adjusted PY benchmarks. Net savings to CMS were $694.6 million (2.6%), and the net savings to ACOs were $948.4 million (3.4%) compared to model benchmarks. These results reflect significant gains from the previous year, where net savings were reported at $371.5 million for CMS and $484.1 million for ACOs, demonstrating the model’s evolving efficacy and its participants’ improved performance.
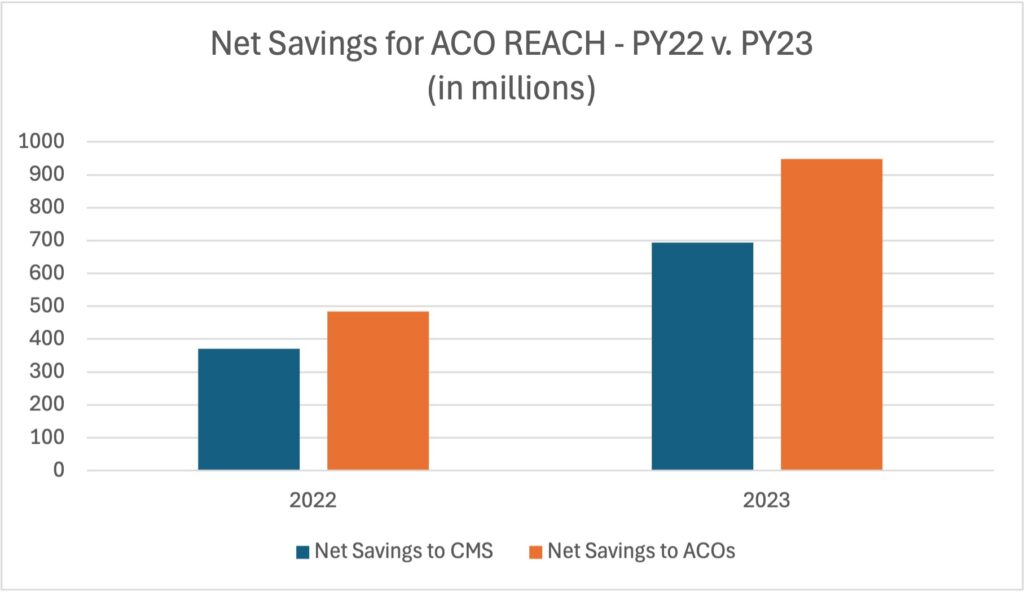
In 2023, 132 ACOs participated in ACO REACH, and 96 (73%) achieved positive net savings through financial settlements. A unique feature of ACO REACH is its dual risk options—Global and Professional—where participants have flexibility in choosing their level of financial risk. This year, 79% of ACOs in the Global risk track and 67% in the Professional track succeeded in generating shared savings, showcasing the program’s adaptability to diverse organizational structures and risk preferences.
Alongside its financial outcomes, ACO REACH focused on advancing quality measures with an emphasis on both claims-based and demographic data reporting. Notably, 32 ACOs achieved a Total Quality Score (TQS) of 100%, with the model-wide average TQS reaching 78.55% for Standard/New Entrant ACOs and 86.73% for High Needs Population ACOs.
With CMS aiming to enhance access to accountable care, the ACO REACH Model has played an essential role in shaping a more equitable and sustainable healthcare landscape, providing valuable insights for similar initiatives like the Medicare Shared Savings Program (MSSP).
Additional Reference: Spreadsheet showing individual ACO results – https://www.cms.gov/priorities/innovation/files/aco-reach-py2022-fin-qual-results.xlsx
Medicare Shared Savings Program (MSSP): Performance Year 2023
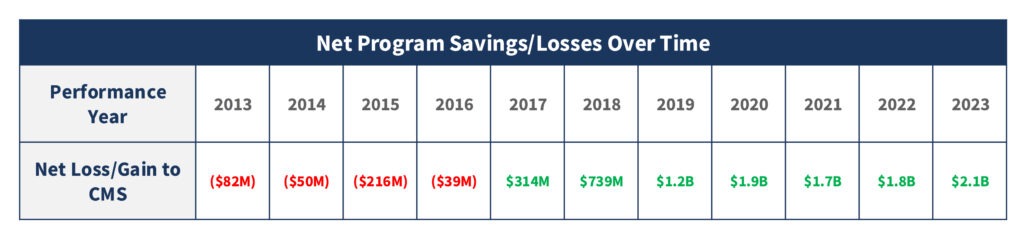
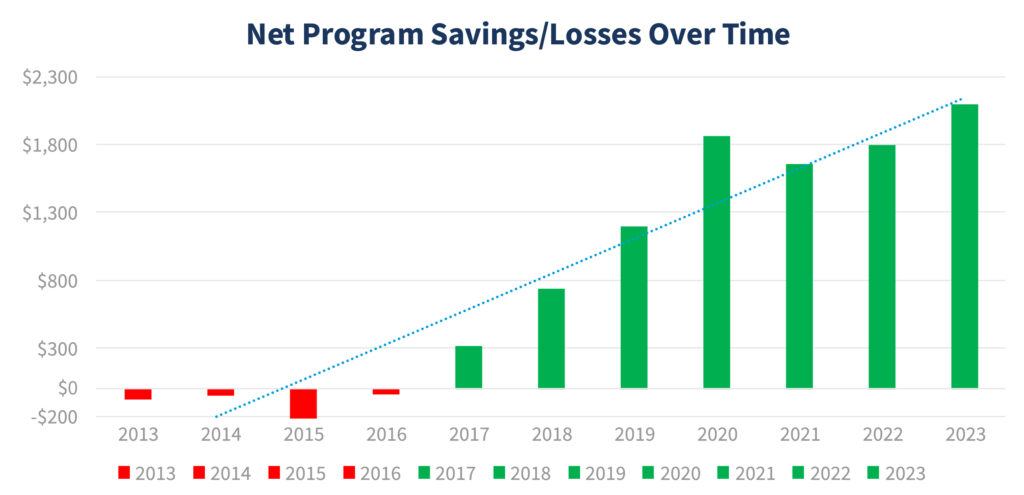
The recent announcement from CMS on the MSSP also marks a major milestone for the value movement. MSSP ACOs, delivered record results in Performance Year 2023. Collectively, MSSP ACOs generated $5.2 billion in total savings, with $2.1 billion retained by Medicare—a testament to the impact of value-based care on both quality for the beneficiary and cost benefiting the taxpayer. The continued success of the MSSP, CMS’s flagship value-based care initiative, has now resulted in seven consecutive years of savings for Medicare—culminating in a record-breaking performance in the latest year.
In 2023, the MSSP included over 500 ACOs, significantly larger than the 132 ACOs participating in the ACO REACH Model. This scale allows the MSSP to generate considerable savings, totaling $5.2 billion, with $2.1 billion retained by Medicare, illustrating the collective impact of value-based care on healthcare costs and outcomes.
The savings in 2023 were largely driven by the performance of low-revenue ACOs, which generated a net savings of $248 per Medicare beneficiary per year on average. Primary care-driven ACOs within this group performed even better, achieving net savings of $319 per capita, more than double the savings of high-revenue ACOs. This performance differential demonstrates how the ACO model, especially when led by primary care physicians as the care quarterback, is successfully delivering on its promise to transform care while managing costs for Medicare beneficiaries. Overall, the consistent and sustained success of the MSSP is a testament to how value-based care is working to transform the healthcare landscape over time. The Medicare Shared Savings Program’s results illustrate that value transformation requires patience and persistence to yield the richest rewards in care quality and cost efficiency. In part to this success, is that many organizations look to partnerships that offer specialized expertise, technology, and operational support to streamline their transition.
Additional Reference: Spreadsheet showing individual ACO results – https://data.cms.gov/medicare-shared-savings-program/performance-year-financial-and-quality-results/data
The Highs—and What’s Still Missing—in Value-Based Care
At Lumeris, we’re inspired by the efforts of our peers who have taken bold steps to improve healthcare quality and efficiency. This year’s success for both the ACO REACH and MSSP programs points to the power of accountable care in driving improved outcomes, especially in areas like diabetes and blood pressure control, cancer screenings, and preventive health measures. The consistent performance of ACOs with high-quality scores demonstrates that coordinated, patient-centered care can address pressing health challenges. The results reinforce our commitment to advancing this model with a holistic approach, focusing on outcomes that matter to patients and providers alike.
The success of ACO REACH and the MSSP is undeniable, yet there’s more to be done to achieve the full potential of value-based care. The current model has proven to be a strong foundation, but its growth and scalability require strategic improvements. Here’s where we see the gaps and opportunities:
- Primary Care as the Backbone
Primary care-led ACOs continue to achieve higher per capita savings than their counterparts. This makes sense, as primary care providers are positioned to focus on preventive care, coordination, and population health management—all essential components of value-based care. Unlike ACOs that also manage high-cost acute care assets, primary care-focused ACOs benefit from an operational model that avoids the complexities of balancing a dual business model. This allows them to position care delivery with a singular focus on setting the right care in the right place at the right time, creating a more streamlined and effective approach to improving patient outcomes and reducing costs. At Lumeris, we recognize that to sustain these gains, health systems need to further integrate primary care with other specialties through better data sharing, realigned incentives, and performance accountability. In some cases, it may even mean redirecting certain patient attributions—such as assigning step 2 attribution from cardiologists back to primary care physicians, who often have a more comprehensive view of all a patient’s health conditions. Furthermore, we believe that advancements in artificial intelligence will be the only way to automate and scale primary care such that health systems can effectively meet the growing demands of their patient populations in the future. - Leveraging Data for Continuous Improvement
Quality improvements in chronic disease management and preventive screenings are encouraging signs, yet many organizations lack the advanced data infrastructure needed for ongoing optimization. Effective data sharing, transparency, and robust analytics enable providers to proactively manage high-risk patients and prevent unnecessary hospitalizations. Lumeris helps ACOs move beyond basic reporting by offering AI-driven predictive analytics and actionable insights that allow for real-time adjustments to care pathways and produce actionable interventions. Lumeris’ advanced analytics capabilities not only highlight gaps but also enable ACOs to make the necessary changes to meet or exceed quality benchmarks. - Expanding Access to Underserved Communities
While the MSSP and REACH ACOs’ results reflect an overall improvement in quality, many underserved communities still face barriers to accessing high-quality, affordable care. Lumeris believes in a model that addresses social determinants of health (SDoH) alongside clinical care, recognizing that access challenges often contribute to health disparities. With the help of CMS’s continued support, we assist organizations in implementing SDoH data solutions to target interventions for these communities, improving accessibility and outcomes where it’s needed most. - Encouraging Digital Quality Measurement
As CMS moves toward electronic clinical quality measures (eCQMs), transitioning MSSP ACOs must transition to digital quality measurement as a basis to further improve health outcomes and efficiencies. Although nearly double the MSSP ACOs have adopted eCQMs compared to last year, many still face technical and resource-related barriers. Lumeris supports the shift to digital by providing ACOs with the necessary tools and expertise to streamline data collection and reporting, helping provider organizations prepare for CMS’s evolving requirements. - Sustaining and Scaling Value-Based Care Participation
Although the MSSP is growing, current participation still falls short of CMS’s goal to have all Medicare beneficiaries in accountable care arrangements by 2030. This goal is further challenged by the fact that ACO REACH is expected to conclude by December 2026 and a successor model has not been announced yet. To achieve this critical mass, the industry must continue to incentivize and support new entrants, particularly health systems that may lack the resources to transition to value-based models. Lumeris offers solutions tailored to help these organizations join and succeed in ACO models, allowing for scalable impact and sustainable growth.
Looking Ahead: Consider Realizing the Full Potential of Value-Based Care
While these performance results from ACO REACH and the MSSP show that value-based care is on the right path, achieving the ultimate vision will require collaboration, innovation, and resource support. At Lumeris, we are committed to guiding healthcare organizations through this journey, providing the tools, insights, and partnerships needed to unlock their full potential. Our expertise in population health management and comprehensive value-based care solutions enable ACOs to not only meet but exceed CMS’s goals for quality and savings.
As the Medicare ACOs continue to evolve, let’s keep the momentum going. We commend the ACOs that have laid the groundwork for a more sustainable and patient-centered model of care. Building on a solid foundation of value-based success, Lumeris is focused on transformation at scale. We partner with leading health systems and physician practices across the country and, together, we are advancing the aims of value-based care through technology-driven insights, care coordination, and streamlined processes.
Ready to take the next step in your ACO’s journey? Contact us to learn how Lumeris can help you transform your organization for sustainable, value-based care success.