A high-functioning health system needs a strong focus on both primary and specialty care population-based models. Additional understanding of the depth and scope provided by specialty care is essential to effective coordination between specialty and primary care providers. The need for coordination has become more pronounced given the annual average number of specialist visits have increased by 20%. In a publication released by the Centers for Medicare and Medicaid Services (CMS) in June, the average number of specialists that a primary care provider coordinated with increased from 52 to 95 physicians—an 83% increase since 2000.[1]
The growth in specialty care coordination with primary care has played in overall medical spending. From 2002-2016[2], the total annual health care spending increased by $806 billion. Of that spend increase, specialists accounted for 18%, while primary care accounted for only 4%. What these studies have demonstrated is the inherent need for reigning in excessive or unnecessary specialty care medical costs. Indeed, this was CMS’ intent with the Oncology Care Model (OCM), and ultimately, the new Enhancing Oncology Model (EOM).
Lessons Learned[3], from the Oncology Care Model
The OCM was launched in 2017, with around 200 practices representing around 3,200 oncologists and 150,000 unique beneficiaries receiving chemotherapy. Payment for participating groups involved the standard fee for service (FFS) billing with an additional Monthly Enhanced Oncology Services (MEOS) payment. This required a mechanism to identify and track eligible patients for the six-month episode of care and the chemotherapy trigger date.
Key elements of success in OCM:
- An oncology-focused Electronic Health Records (EHR)
- Infrastructure for 24/7 patient access to both clinicians and EHR
- Use of claims and clinical data for cost, quality, and utilization management
- Using evidence-based clinical guidelines to guide care management plans
The program produced several positive outcomes, such as accelerated transition to workflows designed to support value-based care, providers and care teams reporting improved coordination of care, and patient’s reporting higher levels of satisfaction. Quality improvements were acknowledged through higher levels of screening and follow-up care for pain and depression.
Total Episodes of Care (TEC) expenditure improvements were notable for lung cancer, colorectal cancer, lymphoma, and high-risk breast cancer. In comparison to: an overall rate of increased TEC expenditures for non-OCM patients.
Some notable feedback from the OCM participants highlights the need to:
- Focus on patient-centered cancer care journey
- Improve patient attribution and cancer episode identification
- Deploy oncology-specific clinical analytics
- Find ways to decrease the administrative burden of program participation
The OCM was a useful experiment to identify challenges in implementation and execution of an oncology managed care model. It highlighted operational, financial accounting, infrastructure investment, and time requirements that should be taken into consideration when evaluating future oncology model participation. Further, it demonstrated that focusing on a select TEP diagnosis, rather than all cancer diagnoses, may result in improved financial performance.
The initiated projects that The Centers for Medicare and Medicaid Innovation (CMMI) focused on specialty care have shown substantive promise and value – examples of this includes the Comprehensive Care for Joint Replacement Model, ESRD (End Stage Renal Disease) Treatment Choices Model, and the Oncology Care Model.
Built on the success and learned lessons from the OCM, CMMI announced the EOM in June of 2022.
What the New EOM Means to Provider Groups
The new, five-year voluntary episodic oncology model builds off the lessons learned from the Oncology Care Model, which ended in July 2022. Under EOM, Provider Group Practices (PGP) will have the option to participate under two available risk arrangements containing a difference of minimal and nominal downside risk.
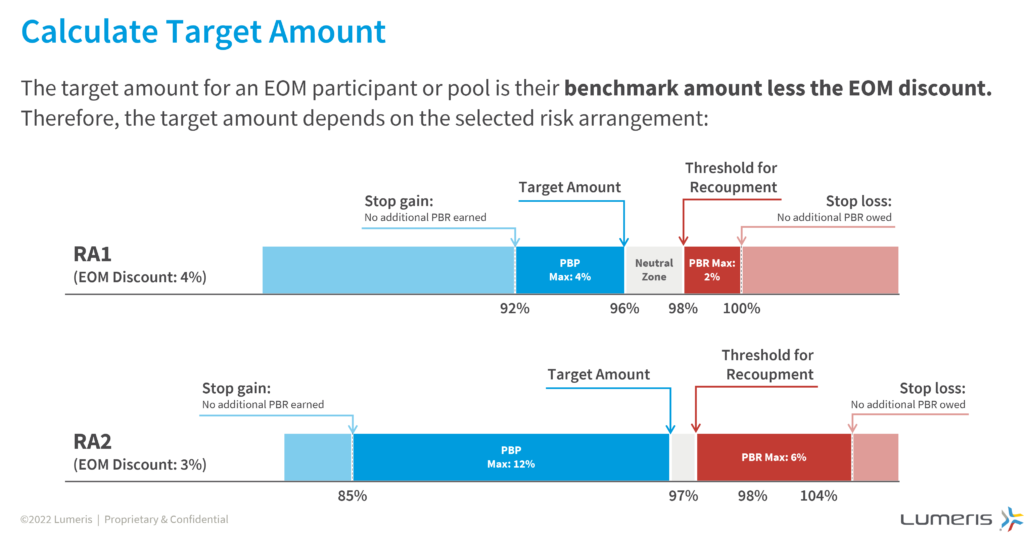
At the start of the first performance period beginning July 1, 2023, participating groups are responsible for the total cost of care and quality for fee-for-service Medicare beneficiaries receiving systematic chemotherapy across seven high-risk cancer types. Each cancer episode of care lasts a duration of six months, and during that period, PGPs have the option to bill monthly enhanced oncology payments of $70 for each beneficiary (an additional $30 for Dual eligible patients) if certain services are provided by the PGP. At the end of each performance period, participants may earn a performance-based payment (PBP) or owe the Centers for Medicare and Medicaid Services (CMS) a performance-based recoupment (PBR) if cancer episode expenditures exceed their expected target price. The amount of refund or performance payment is determined by the risk arrangement selected by the participant group.
If you are an oncology practice or a multi-specialty group with oncology physicians providing care to beneficiaries with breast, leukemia, lung, lymphoma, myeloma, prostate, or colon cancer and are interested in applying before the October 10th deadline[4], here are other things to consider:
Summary of Episode Structure: Generally, an episode is triggered under the model when a patient receives an “initiating cancer therapy” or chemotherapy claim. The episodes are then attributed to the participating oncology provider with the first evaluation & management service. For the next six months, beneficiary expenditures under Medicare Parts A, B, and certain D payments, and at this time is when participants may begin billing MEOS payments.
Retrospective reconciliation: As previously mentioned, at the end of the performance period, CMS conducts a retrospective reconciliation by tabulating actual expenditures for each episode and comparing against predicted episode expenditure benchmark for each cancer type. A PBP or PBR is determined, and the amount received or owed to CMS is adjusted by a geographic factor and quality score performance. See Figure 2 above. Note that PGP groups may elect for an individual reconciliation or “pool” their performance with other groups.
Meanwhile, to engage other providers impacting the quality and cost of care for beneficiaries, PGP participants may enter into financial sharing arrangements with other providers referred to as “Care Partners.” This allows the opportunity for the extended network of care continuum team members to be incentivized to follow compliantly designed care plans.
- Considerations for those interested in EOM:
- Drive and expand patient-centered goals that align with other oncology certification programs
- Improve cancer care experience using electronic Patient-reported Outcome Measures (ePROMs) shared decision making
- Incorporate MEOS payment revenue to support care management investments
- Opportunity to qualify as Merit-based Incentive Program Alternative Payment Model designation or an Advanced Alternative Payment Model Qualified Provider in the CMS Quality Payment Program
- Acquire access to claims data to which enables visibility into the patient care journey to deploy higher quality interventions in a faster response time
- In a highly competitive market with others participating in EOM, you can defend against encroaching oncology alignment and referral redirection
- Prepare for potential future mandatory models incorporating oncology episodes
[1] Pathways for Specialty Care Coordination and Integration in Population-based Models. CMS, June 17, 2022.
[2] Data from the Medical Expenditure Panel Survey, 2002-2016 (https://www.meps.ahrq.gov/mepsweb/)
[3] Reflections on the Oncology Care Model and Looking Ahead to the Enhancing Oncology Model. ASCO, September 2022.
[4] Applications due 10/10/22 for a 7/01/23 start
[5] Enhancing Oncology Model Payment Methodology Webinar, July 2022.