The statements contained in this analysis are solely those of the authors and do not necessarily reflect the views or policies of CMS. The authors assume responsibility for the accuracy and completeness of the information contained in this document.
PART 1: Understanding the programmatic health equity components
As the CMMI (Center for Medicare & Medicaid Innovation) Direct Contracting Program transitions to the ACO REACH Model in PY2023, many in the market have asked: “what has changed?” One notable change is the inclusion of one of the core tenants of the CMMI Strategic Plan announced last year to have Health Equity as a central component of all future CMMI models.
In Part One* of this two-part series, Lumeris and CareJourney have partnered to help current Direct Contracting Entities prepare for their transition to ACO REACH, as well as ACO REACH applicants planning to participate in 2023 gain a better understanding of the key Health Equity components in the ACO REACH Model. These four components are summarized as:
- Embed Health Equity into Benchmark: The Health Equity Benchmark Adjustment
- Address Health Equity in Risk Adjustment: The Consideration of the Demographic Relative Factors Component of Risk Scores
- Improve Data Collection across Communities: Collecting patient reported demographic and social determinants of health data to better understand beneficiaries and communities with more accurate data.
- Ensure Accountability of Addressing Health Inequities: Develop and abide by Health Equity Improvement Plans
While Part One is to help prospective REACH ACOs “Understand”, Part Two will be subsequently released to help “Plan” and take “Action” on addressing the needs of the disadvantaged or underserved populations that CMMI and the broader provider community is looking to serve.
To begin, understanding how CMMI and CMS defines “Health Equity” and “Underserved Communities” will help ACO REACH participants prepare for the Health Equity components of the model.
“As defined in the Racial Equity and Support for Underserved Communities Through the Federal Government Executive Order 13985, the term “equity” means “The consistent and systematic fair, just, and impartial treatment of all individuals, including individuals who belong to underserved communities that have been denied such treatment, such as Black, Latino, and Indigenous and Native American persons, Asian Americans and Pacific Islanders and other persons of color; members of religious minorities; lesbian, gay, bisexual, transgender, and queer (LGBTQ+) persons; persons with disabilities; persons who live in rural areas; and persons otherwise adversely affected by persistent poverty or inequality. The term “underserved communities” refers to populations sharing a particular characteristic, as well as geographic communities, that have been systematically denied a full opportunity to participate in aspects of economic, social, and civic life, as exemplified by [the aforementioned list.]”
–CMMI Strategy Refresh, October 2021
Embed Health Equity into Benchmark: The Health Equity Benchmark Addition
Starting in PY2023, CMS will identify underserved beneficiaries using a composite measure comprised of both the Area Deprivation Index and Dual Medicaid Status, incorporating this into the ACO REACH benchmark methodology.
Methodology Components
- Area Deprivation Index (ADI): ADI captures local socioeconomic factors correlated with medical disparities and being underserved (Income/Employment, Housing, Education, Household Characteristics). ACO REACH is utilizing ADI as a national percentile, scored 0-99 comparing census block groups to one another across the U.S.
- Dual Medicaid Status: Whether or not a beneficiary has Dual Medicaid Status (dual-eligible) captures economic challenges directly affecting the individual beneficiaries’ ability to access care
Individual Beneficiary Benchmark Calculation
- CMS will calculate the benchmark adjustment starting with the national ADI score for a beneficiary’s census block group and applying a 25-point increase for dual-eligibles
- Ex: a dual-eligible beneficiary residing in a census block group in the 65th percentile would be calculated: 65 + 25 = 90
- CMS then stratifies aligned beneficiaries based on the composite score, identifies the top decile (top 10%) for an upward adjustment ($30 PBPM) and bottom 5 deciles (bottom 50%) for a downward adjustment ($6 PBPM)
ACO Net Benchmark Calculation
- Each ACO receives a net benchmark adjustment based on the number of aligned beneficiaries in each category
- Ex: an ACO with 50 beneficiaries in the top decile and 250 beneficiaries in the bottom five deciles in a given month would receive [($30 PBPM x 50)] – ($6 PBPM x 250)] = 0
- CMS suggests that most ACOs will be marginally affected by this adjustment; within +/- 0.2% impact on the PY benchmark**
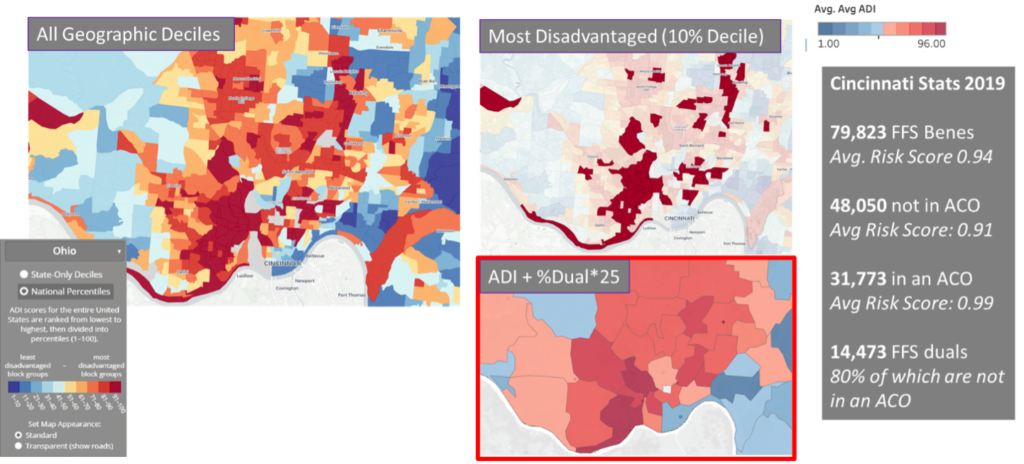
Utilizing a tangible, localized example of this Health Equity Benchmark Adjustment in action, Cincinnati, Ohio, is represented below. The map on the left shows ADI census block groups in the Cincinnati area color coded according to which decile they belong to, with the darkest red correlating to the most distressed areas. These areas are further highlighted in the top right-side map. The map on the bottom right illustrates the ACO REACH methodology by multiplying the percent of beneficiaries that are dual eligible times twenty-five and adding that product to the ADI score, again utilizing a heat map and the darkest red color to illustrate the tenth decile. The National ADI can be publicly observed for your community via the University of Wisconsin Center for Health Disparities Research Neighborhood Atlas.
Address Health Equity in Risk Adjustment: The Incorporation of the Demographic Risk Score
Beginning in PY2024, a symmetric risk score growth cap will continue to be applied but will be adjusted relative to an ACO’s independently calculated demographic risk score growth and will have a notable effect on the risk adjustment methodology. The risk score will now have both demographic relative factors and disease relative factors. The four factors that make up demographic relative risk are the following:
Please take note that:
- While we await final guidance from CMMI on specifics regarding ACO REACH risk score calculation, we anticipate that for Standard and New Entrant ACOs, risk scores will be calculated in the same manner as for Direct Contracting and Medicare by utilizing the 2020 CMS-HCC risk adjustment model, or Version 24 (v24). The demographic relative factor component of the HCC risk score is found in table VI-1 of the Medicare Advantage Advance Rate Notice.
- Through directly linking the application of the risk score growth cap to the ACO-level independently calculated demographic risk score growth, the cap is intended to better account for changes in beneficiary health status beyond the +/- 3% threshold. Older beneficiaries and dual eligible beneficiaries each have higher demographic relative factors as compared to younger, non-dual eligible beneficiaries.
- An example of how the symmetric cap and demographic adjustment will be reflected under the new methodology is referenced in the table below:
RY* Risk Score (HCC) | PY Risk Score (HCC) | HCC Risk Score Growth | Demog. Risk Score Growth | Capped Current Risk Score | Demog.-Adjusted Capped Risk Score |
1.0 | 1.1 | +10% | +2% | 1.03 (+3%) | 1.05 (+5%) |
1.0 | 1.1 | +10% | -1% | 1.03 (+3%) | 1.02 (+2%) |
| 1.0 | 0.9 | -10% | +3% | 0.97 (-3%) | 1.0 (+0%) |
Reference Year*
Table Source: “ACO Realizing Equity, Access, and Community Health (REACH) Model Financial Methodology Updates Webinar” presented by CMS/CMMI on March 28, 2022
Improve Data Collection Across Communities: Incorporating Market and Community-level Indicators
REACH ACOs will be required to collect beneficiary reported demographic data to both support further awareness of community-based inequities and also monitor the impact the interventions available in programs like ACO REACH will have on these communities. Beneficiary reported demographic data is the gold standard for understanding how demographics contribute to a patient’s health outcomes, but has not historically been collected and aggregated. This data collection requirement includes acquiring the following data fields (beneficiary self-reported):
- Race
- Ethnicity
- Language
- Gender identity
- Sexual orientation
Currently, CMS has offered two options for submission:
- CMS questionnaire using FHIR data standard
- Excel template provided by CMS
In addition, CMS is considering rewarding ACOs for successful reporting, such as a bonus to the ACO’s Total Quality Score up to an additional 10 percentage points (no downward adjustment if not submitting data).
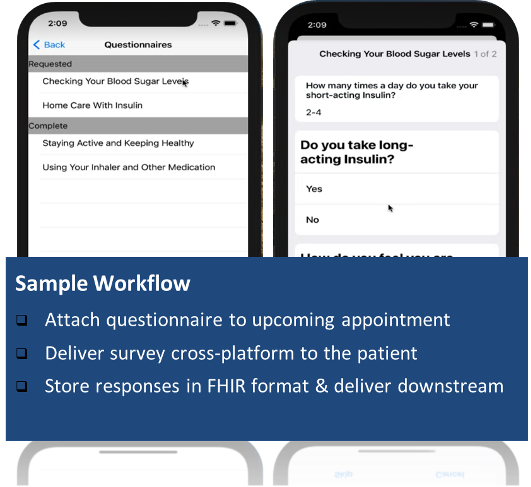
One example approach for consideration is to consider the following sample workflow***:
Ensure Accountability of Addressing Health Inequities: Form and abide by Health Equity Improvement Plans
Beginning in PY2023, all ACO REACH participants will be required to submit and execute a Health Equity Plan (HEP) at the beginning of each performance year. The current expected due date for REACH ACOs to deliver the plan to CMS is March 2023 (subject to change).
Later this summer, CMS will release a template with more detailed guidelines for the HEP. This template is expected to align to the CMS Disparities Impact Statement – which is summarized as:
- Identify health disparities and priority populations
- Define short- and long-term goals
- Establish the organization’s health equity strategy
- Determine what your organization needs to implement its health equity strategy
- Monitor and evaluate progress
In the meantime, CMS is encouraging ACOs to identify community partners and integrate these community partners into the Health Equity Plan.
Thus, there are several opportunities for providers to continue the pursuit of helping underserved communities in their service areas. Some opportunities to consider:
- Leverage this program to expand on your existing local mission’s intent to be the community caregiver of choice and deliver services to the community (with supported funding beyond grants)
- If Not-for-Profit, utilize the Community Needs Assessment efforts beyond use for maintaining non-taxable status
- Develop the plan of action to inform care, social, and community worker-support teams to improve the health of the underserved communities.
About CareJourney
CareJourney was founded in 2014 under the belief that our nation’s transition to value-based care is an important one, but without an “operating manual” that can reliably deliver on the promise of better quality at a lower cost. Our mission is to empower individuals and organizations they trust with open, clinically relevant analytics and insights in the pursuit of the optimal healthcare journey.
To learn more about CareJourney, please visit www.carejourney.com
*Part One was presented at the America’s Physicians Groups’ Annual Meeting Pre-Conference, June 1, 2022
**Source: “ACO Realizing Equity, Access, and Community Health (REACH) Model 1 Request for Applications 02/24/2022” released by CMS/CMMI in February 2022
***Open source app now available on GitHub ResearchKitOnFHIR

